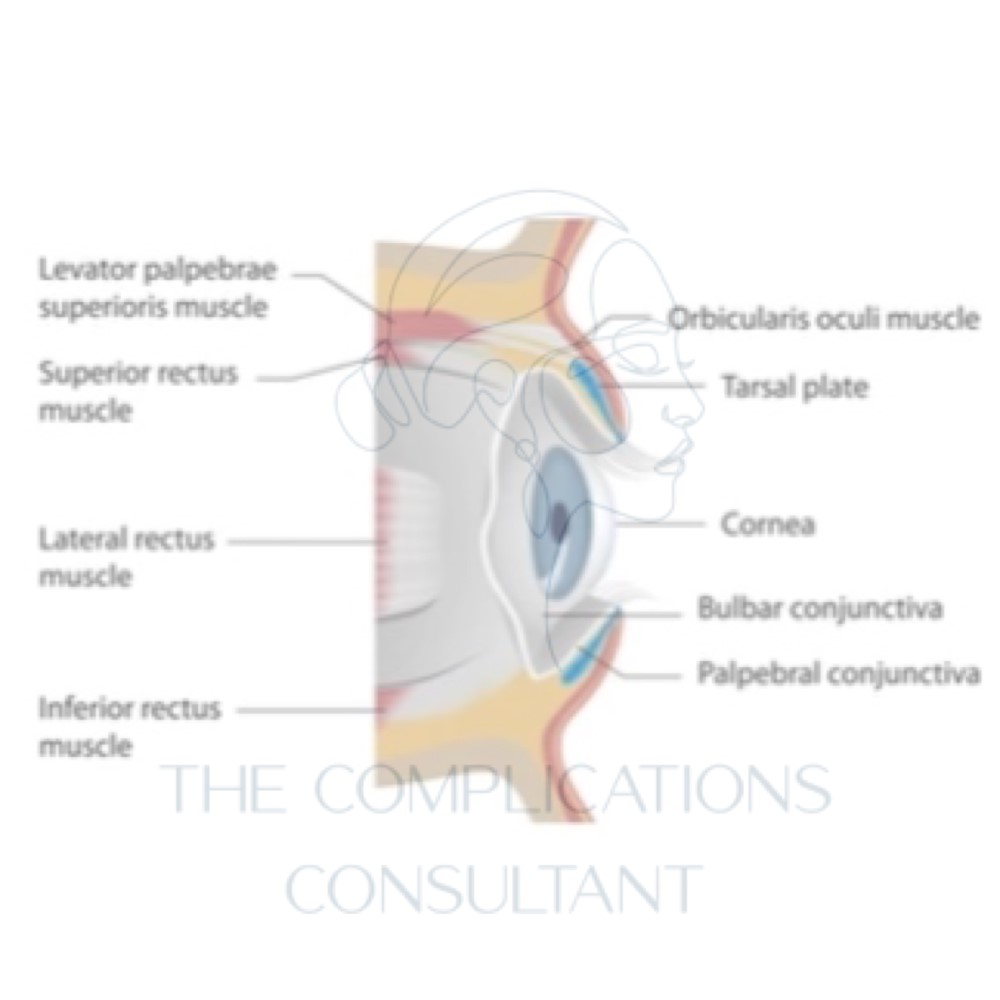
Anatomy of the Eye; muscles that elevate the eyelid
It is always wise to have to hand or within visible reach, a 3D model of the anatomical structures you are injecting. This will help you visualise the anatomy and be an all-round safer injector. The benefit of having a 3D understanding of a structure most viewed as 2D is vast.
Making understanding of the depth of the muscles, for example, that lift the eyelid are far deeper into the orbit than the textbooks depict. Armed with such knowledge, you very soon realise that it isn’t the injecting proximity to the eyelid that is important, but the placement of toxin within the orbit that is.
Muscles that elevate the eyelid
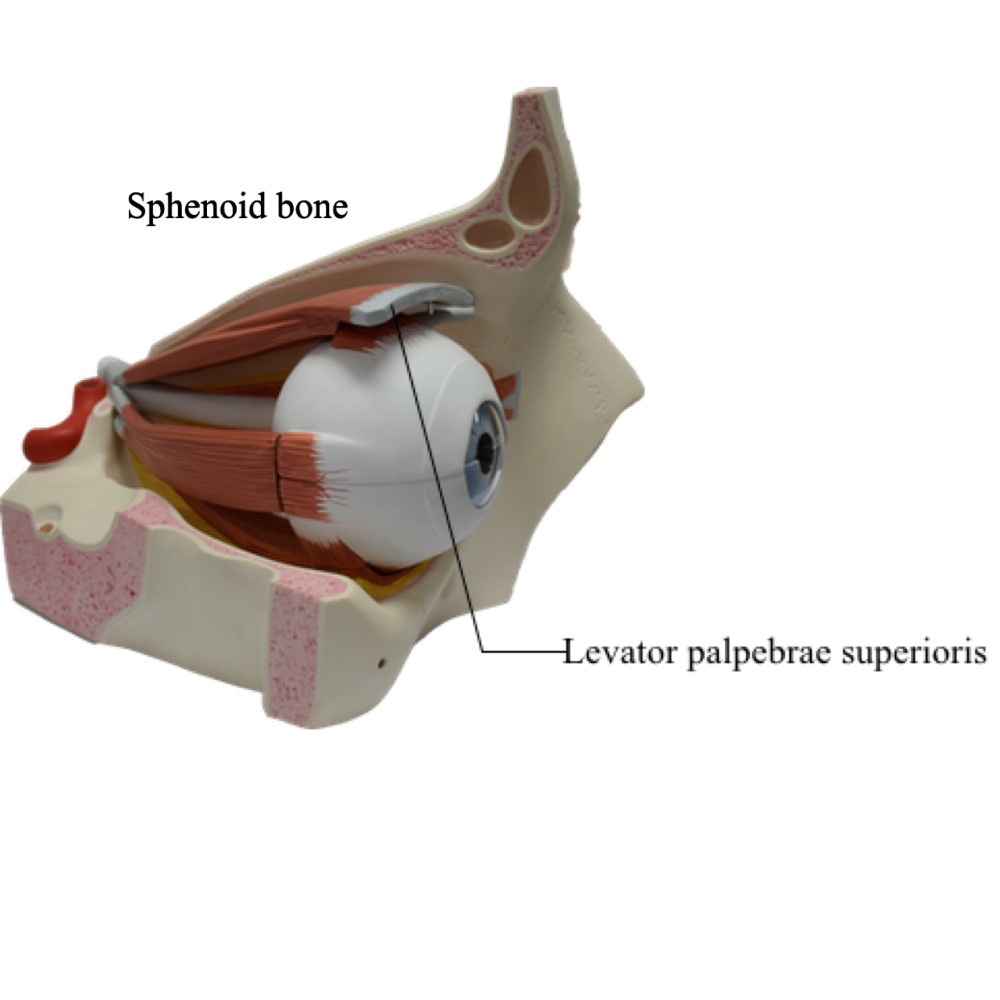
LEVATOR PALPEBRAE SUPERIORIS
- Originates from the sphenoid bone
- Slightly superior to the optic foramen
- Becomes wider, thinner and more fibrous the further forward it sits
- It then becomes levator aponeurosis
- This attaches to the skin of the eyelid and tarsal plate
- Attention to nerve damage must also be paid when injecting
- Nerve innovation is by somatic (consciously controlled) nervous system
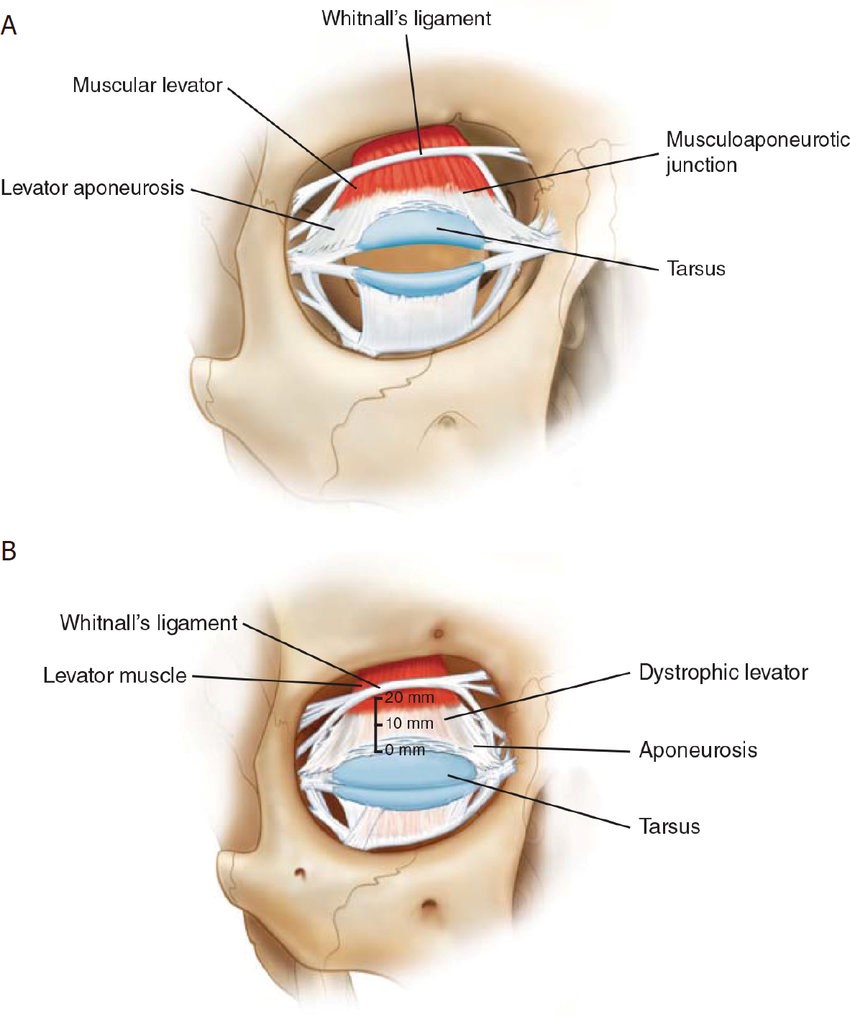
SUPERIOR TARSAL MUSCLE
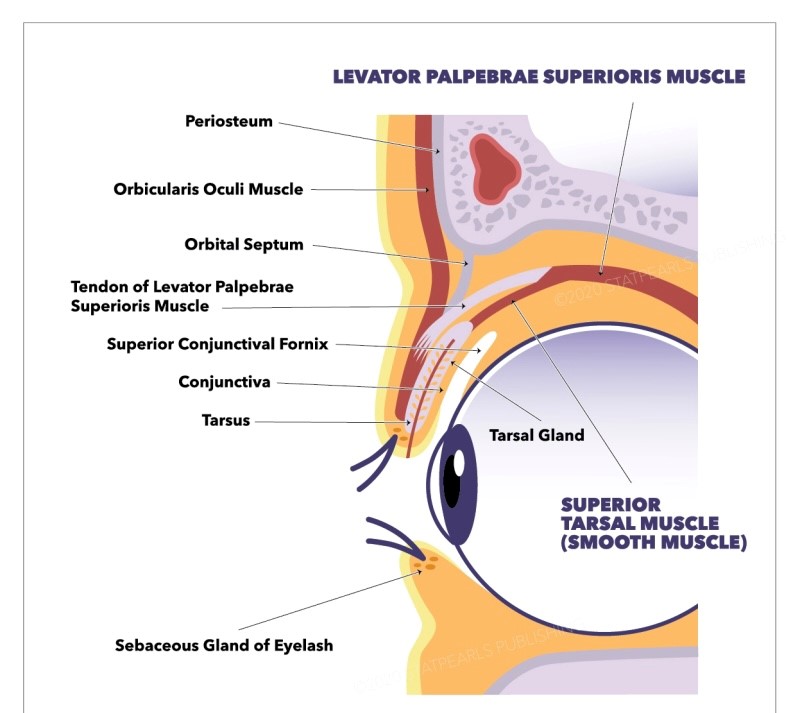
- Lies within the lid in front of the levator palpebrae superioris
- Behind it lies the superior tarsal muscle
- As you can see in the photo this is smooth muscle
- Innovated by sympathetic nervous system
- Becomes weaker when exposed to botulinum toxin
- Can contract unlike levator palpebrae superioris
Understanding this enables the understanding of the different modes of action of eyelid ptosis. Botulinum can enter the orbital anatomy and effect both muscles or just one.
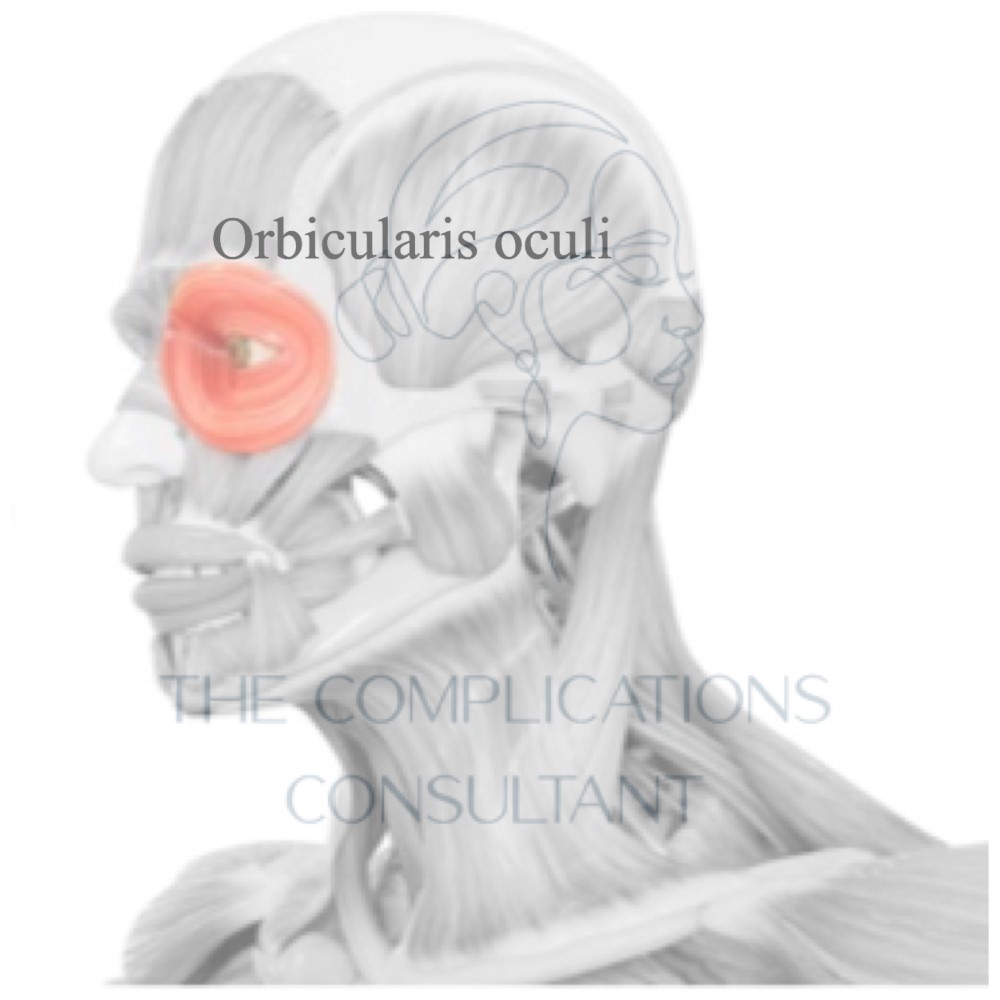
LAYERS OF TISSUE THE NEEDLE MUST PASS THROUGH FOR THIS TO OCCUR; skin, hypodermis, orbicularis oculi and orbital septum.
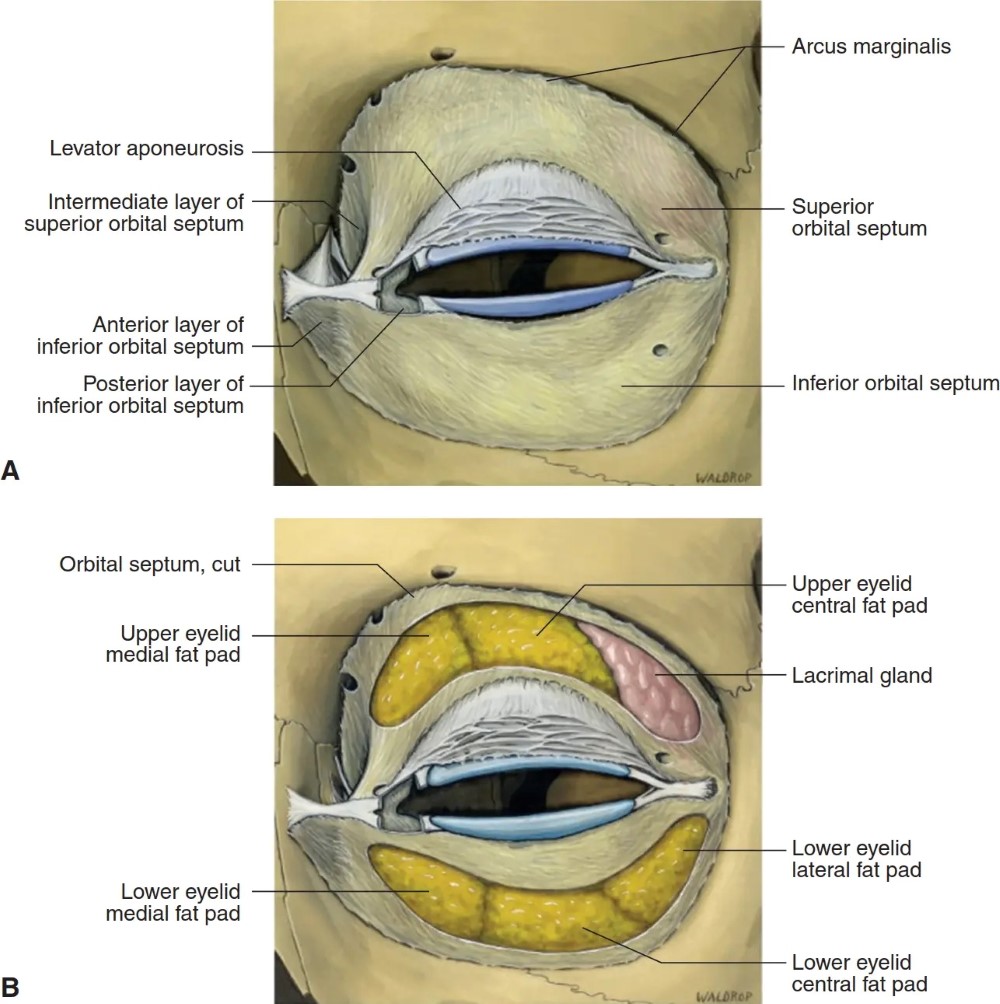
Due to the anatomical structure of the orbital septum being semipermeable with perforations, it can allow the passage of supratrochlear and supraorbital nerves, arteries and veins to the forehead.
Although instinctively you will attribute eyelid ptosis after treatment to the botulinum that has been injected, it is worth considering other possible causes like cranial nerve pathology or damage to the sympathetic nerve supply. This is known as Horner’s syndrome and can occur with lung cancer for reasons unknown.